The earliest possible indication of abnormalities allows for the earliest possible intervention.
Thermography is unaffected by breast density, breast implants or scars from surgery. There is no contact, no harmful radiation, and no contraindications – it is as simple as standing in front of a camera.
What Does Breast Thermography Detect?

Breast thermography detects the physiological changes in the breast tissue that correlate with cancerous or pre-cancerous states. Cancers, even in their earliest stages, need nutrients to maintain or accelerate their growth. To provide nutrients and oxygen to a growing abnormality, blood vessels are caused to remain open, inactive blood vessels are activated and new ones are formed, in a process called neoangiogenesis. This vascular process causes the surface temperature to increase in the affected regions, which is seen using infrared imaging cameras. Additionally, the newly formed or activated blood vessels have a distinct appearance which thermography can detect.
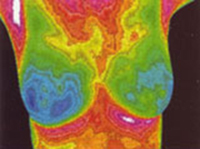
Thermography is a physiological test. Therefore, it cannot identify tumors, but it does provide the clinician with extremely useful information regarding areas of abnormality which can be examined clinically and with anatomic tests. By the time a tumor has grown large enough to be detectable by physical examination or mammography; it has in fact been growing for several years, doubling in size more than 25 times from the original malignant cell colony. Since thermal imaging detects changes at the cellular level, studies suggest that this test can detect activity – such as neoangiogenesis – eight to ten years BEFORE any other test. Thermography affords us the unique opportunity to view the physiological changes that occur BEFORE the actual formation of the tumor.
What’s Included in the Breast Scan?
- Bilateral imaging of the breasts in multiple positions
- Early detection of thermal asymmetries, vascular activity, and lymphatic congestion
- Useful for preventive screening, monitoring fibrocystic or dense breasts, and post-surgical follow-up
- Safe for all ages—no radiation or compression
Each exam is reviewed by a Board-Certified Clinical Thermologist. A written report is provided via email, typically within 2–3 weeks. A phone consultation is optional and can be arranged upon request.
View a Sample Thermal Breast Imaging Report Visit our Fees page for complete pricing and discounts on combined scansIs Thermography Safe?
Breast thermography is a non-contact test. Conversely, mammography involves placing the breast between two plates and subjecting the breast to painful compression. The recommended force used to compress breast tissue in a mammogram is 300 Newtons, the equivalent of placing a fifty-pound weight on the breast. In 1992, an opinion was offered that such compression might lead to distant and lethal spread of malignant cells by rupturing small blood vessels in or around small, as yet undetected, breast cancers.
Breast thermography has been determined to have an average sensitivity and specificity of 90%, and when used as part of a comprehensive, multi-faceted approach, can lead to early detection of 95% of early-stage cancers. This increases the long-term survival rate by as much as 60%.
Click Here to Learn More About the Safety of Thermography
